Debating Ideas is a new section that aims to reflect the values and editorial ethos of the African Arguments book series, publishing engaged, often radical, scholarship, original and activist writing from within the African continent and beyond. It will offer debates and engagements, contexts and controversies, and reviews and responses flowing from the African Arguments books.
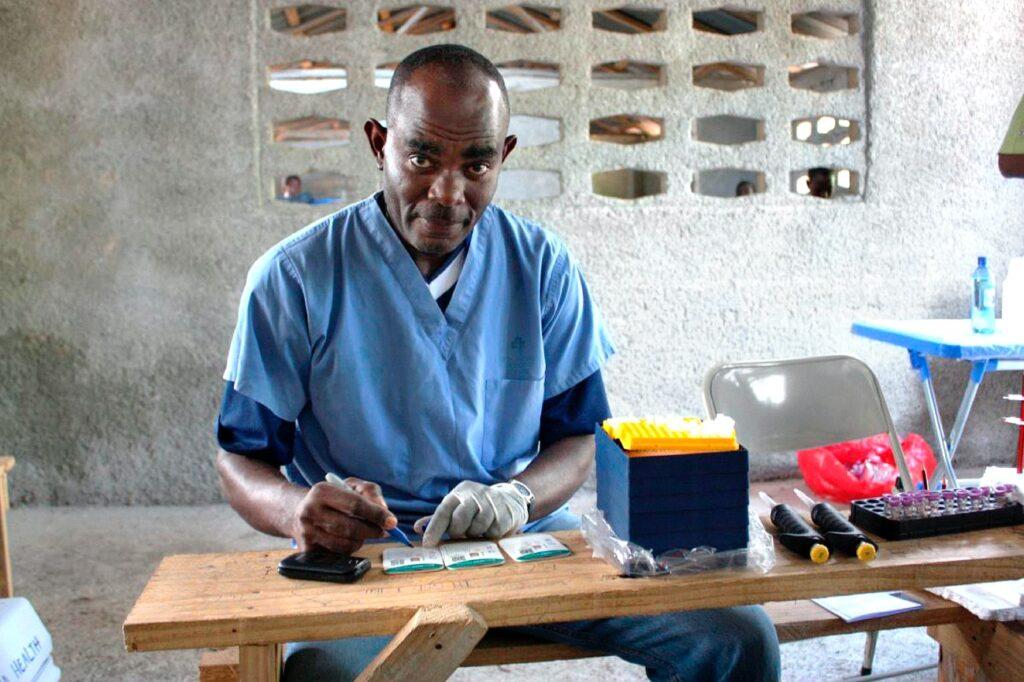
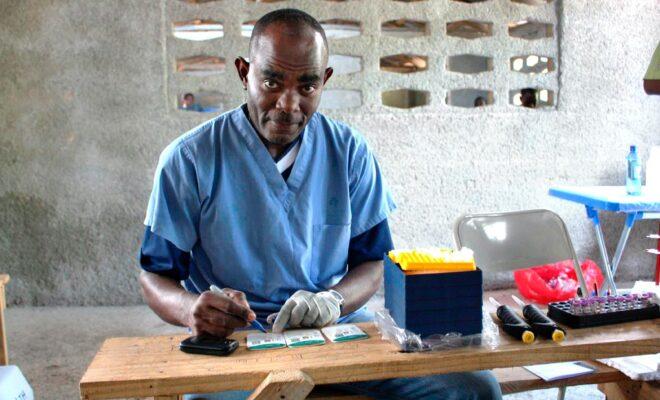
Local health centres experimenting with coronavirus. Source: US Government department: Public Health Image Library, Centers for Disease Control and Prevention
The history of endemic diseases, epidemics and pandemics in Africa shows, contrary to a stubborn belief, that the continent has had a long experience of biomedicine – its theory, techniques, and modes of action. Africans have been active in biomedicine, exercising methods of appropriation and implementation that are as ‘modern’ and effective as in the rest of the world. Like Westerners, they have a long experience in the theories of microbial contagion and modern prophylaxis and treatment, which appeared in the 1860s but did not become widespread until the turn of the twentieth century in Europe, coinciding with colonial expansion across Africa. During and after this period, Africa played an essential role in the discovery and treatment of many diseases such as malaria, trypanosomiasis (sleeping sickness), smallpox, syphilis, tuberculosis and plague (Packard 2007; Webb 2013). Major scientific institutions such as the Pasteur Institute in Paris (1887) and the London School of Hygiene and Tropical Medicine (1899) played a part in circulating imperial knowledge. Their role in the progress of research is increasingly studied by historians (Arnold 1996; Tilley 2012). The expertise of Africans, whether as researchers, caregivers, or ordinary consumers of biomedicine, is therefore comparable to that of the rest of the world. In many points, it is even superior; I will come back to this in my conclusion.
Biomedicine, epidemics, and colonial prejudices
The spread of biomedicine in Africa did however take place in an oppressive colonial context, providing the colonial regime with some of its most effective instruments of control: displacement of populations, cordons sanitaires, collective diagnoses, forced treatment, fertility and birth control policies, and invasions of the privacy of the body of the colonized peoples (Hunt 1990; Summers 1991; Thomas 2003). Doctors and scientists contributed to colonial biopolitics and social engineering by constructing an image of Africans as ‘collective masses’ deprived of their own individuality. A discourse that naturalized and pathologized ‘native subjects’, in the French colonies and elsewhere, supported these health policies (Gilman 1985). Investment in care, however, remained deficient. Until the 1950s and 1960s, the colonies were under-equipped with medical personnel and equipment. The Africanization of the medical professions was neglected until the last years of the colonial presence. When it did occur, it reinforced the hierarchical domination of European personnel (Iliffe 1998).
The deployment of biomedicine, on the other hand, took place alongside violent attacks on local forms of knowledge and healing practices (Feierman and Janzen 1992; Tonda 2002). The criminalization of healers, the proscriptions against ‘witchcraft’ and ‘witch doctors’, the destruction of technologies of genealogical continuity and collective health (relics, ancestor cults, vernacular therapies) turned biomedicine into a traumatic and destructive experience. These policies forced local forms of knowledge, previously publicly available and endorsed by their communities, underground (Feierman and Janzen 1992; Bernault 2019). But Africans also created original ways of appropriating biomedicine, integrating it into local therapeutic practices, deploying strategies and types of expertise that John Janzen studied in Congo under the name of ‘medical pluralism’ (Janzen and Arkinstall 1978).
Contrary to triumphalist discourses on biomedicine and the eradication of epidemics, colonial medicine made numerous errors in interpretation and treatment. It also helped to create ethnic and racial identities (‘types’, ‘races’, supposed physical and biological traits) that were forcibly assigned to the colonized (Gilman 1985; Arnold 1996). One example is the case of syphilis diagnosed in 1908 in East Africa (Uganda) by British doctors, and studied in the pioneering book by the historian Megan Vaughan (1991: 129-54), now a classic that everyone interested in the field should read. The doctors confused cases of yaws and an endemic and non-sexually transmitted variety of syphilis with the variety prevalent in the rest of the world, which led to them developing a corpus of racial prejudice against the sick. The infection rates of what was taken for syphilis (estimated at 80% of those examined) confirmed, in the minds of the colonists, that Africans were degenerate (a ‘dying race’), prone to immorality in their sexual behaviour. Those who presented themselves spontaneously and requested treatment were accused of a lack of decency and moral sense. Those who refused were treated as ignorant primitives, stubbornly resistant to modern science (Vaughan 1991). It was not until the late 1930s that medicine recognized the misdiagnosis that had, for several decades, stigmatized Africans.
An even bigger tragedy hit Uganda. In 1900, anxious to stop an epidemic of trypanosomiasis that had broken out in the district of Busoga, British doctors quarantined those affected on the spot, displacing hundreds of people considered to be healthy to distant regions in line with the technique of cordons sanitaires (Vaughan 1991; Lyons 1992). At that time, the aetiology and pathogenesis of the disease were still poorly understood, much less its treatment. The doctors failed to recognize that many apparently healthy people were carriers of the parasite and would infect the communities in their new places of forced residence. By the time the epidemic declined, around 1908, it had killed more than 250,000 people in a huge sub-region of the African Great Lakes.
These accidents, more structural than circumstantial, continued until the last years of colonization. Guillaume Lachenal has studied a disaster of similar magnitude in Cameroon in the 1950s: the forced injection of Lomidine, an ineffective and dangerous molecule, administered to thousands of people in order to prevent the spread of trypanosomiasis. In what he calls ‘an anthropology of stupidity’, Lachenal shows the reverse side of the colonial policies of modernization: ‘their racial logics, their coercive apparatus, their essential ineffectiveness, and the element of unreason at the very heart of the project of imposing order on Africa by science and technology’ (Lachenal 2014).
Finally, tropical epidemics made it possible to create an urban model specific to the colonies. Historian Philip Curtin was the first to point out the role of debates on health and medicine in urban segregation projects (Curtin 1985). To protect Europeans from malaria, the medical and administrative authorities ordered the expulsion of African residents and their confinement in reserved dormitory areas, separated by health buffers (non aedificandi or no-building zones) from white areas.
In a few cases, Europeans created dormitory towns away from the old city: Hill Station in Sierra Leone was set up on hills, six miles from old Freetown, in 1901, and connected to downtown by a railroad whose construction started in 1902. The scheme was based on the idea that mosquitoes mostly bit at night: Europeans could work in the city during the day and retire to the hills in the evening. The new station excluded all non-Europeans, wealthy Africans as well as Lebanese from residing on the site (Goerg 1998).
However, other researchers, in particular the German doctor Robert Koch, the discoverer of tuberculosis bacillus, had proposed another solution for malaria: the distribution of quinine to all urban residents, both African and European. This solution was rejected on racial grounds, thus permanently marking the landscape of African metropolises by the implementation of authoritarian policies of racial separation (Cohen 1983). Curtin’s work was followed by a rich crop of urban and epidemiological studies, in particular on plague (Echenberg 2002; Ngalamulume 2008; Bigon 2016). Other diseases linked to the economy and colonial upheavals, such as the industrial epidemics of silicosis and tuberculosis, spread among migrant workers in the diamond and gold mines of South Africa (Packart 1989; McCullock 2012).
The failures of colonial medicine in Africa should not overshadow some very important advances. It is thought, for example, that modern epidemiology has found its most influential model in the Community-oriented Primary Care Centers opened by Sidney and Emilie Kark in Zululand between the 1930s and 1958 (Trostle 1986). Trained in Oxford in the social sciences, this couple, both epidemiologists, developed a new care model focusing on the forms of knowledge and the needs of local communities, and in constant dialogue with these latter. Thanks to the contacts of the Karks and the training they gave to many doctors and researchers who spent time as interns at their Polela clinic, the community centres were a success, spreading to South Africa and the rest of the world, especially in the United States. More generally, the history of the contradictory debates and scientific protocols studied by Helen Tilley in a recent work show that Africa has been one of the major centres of medical advances since the last century (Tilley 2011). Julie Livingston’s remarkable work has given a new turn to the methods of medical anthropology by revealing the silent ravages of the cancer epidemic in Botswana (Livingston 2012).
AIDS and Ebola: expertise, triage and therapeutic sovereignty
I end this overview by looking at two recent and particularly instructive epidemics. The first, the HIV/AIDS pandemic, has marked Africa as the continent with the highest prevalence of the disease. In 2018, 26 million people there were living with the virus, i.e. 68% of the total global HIV-positive population (37.9 million) (UNAIDS 2018). The question of the causes and factors of this prevalence has allowed historians such as John Iliffe, with the aid of epidemiologists, to reconstruct the history of the virus (Iliffe 2006; Pepin 2011). The African prevalence of HIV/AIDS is not based on any cultural, economic and scientific backwardness on the continent, nor is it determined by any particular types of sexual or family behaviour. It can only really be explained by the very history of the virus: around the 17th century, in the forest region of south-eastern Cameroon, one strain of HIV, adapted to the human body, broke away from the SIV (Simian Immunodeficiency Virus) endemic among the great apes of the forest (Iliffe 2006; Pepin 2011). Its low level of circulation increased considerably from the end of the 19th century and the colonial conquest onwards: the health disasters comprised by forced labour, migrations and logging sites, and the intensification of hunting and trade, caused the collapse of individuals’ immune defence systems; the increased mobility of HIV, and genetic recombining, increased its virulence. In the 1980s, the epidemic was already circulating invisibly in the general population – not in a ‘target group’ like homosexuals in California. A frozen blood sample from 1959, collected in Kinshasa during a malaria investigation, contained HIV antibodies. To date, this is the oldest proof of the existence of the virus in the world: unique among the 679 other samples collected during the same campaign, it shows the presence, as yet tiny, of the virus in towns. Twenty years later, still silently and invisibly, the disease has now affected a significant proportion of the entire population of Equatorial Africa (Iliffe 2006).
In the 1980s and 1990s, the virus spread rapidly along trade and road routes in the African Great Lakes, East Africa, and finally in Southern Africa, where government mismanagement between the 1980s and 2005 allowed the largest HIV epidemic in the world to spread.
The HIV/AIDS pandemic provides important lessons on the importance of public and local policies. The role of governments, in particular in the public recognition of the epidemic and the call for international aid, was decisive in curbing the spread of the disease (as with Uganda, and conversely, the failure of South Africa). These policies were based, as in Europe and the United States, on education and volunteering (tests and treatments). Above all, many non-governmental organizations, led by African activists, played an essential role in informing the general public and supporting the sick and their families. The inclusion of citizens and their initiatives have proven to be formidable weapons against the epidemic. Many studies have looked at the experience of the disease from below, in families and public life: it is outside clinics, first and foremost, that people experience the disease and give it meaning (Niehaus 2018). Knowledge of the experience and expertise of patients and their entourage is an essential tool for the prevention and treatment of the epidemic. In Uganda, the epidemic affected 13% of inhabitants in 1986; this fell to less than 6% after the mobilization of the government and Ugandan care associations (Iliffe 2006; Reynolds-Whyte 2014). In South Africa, government negligence was also overcome by pressure from civilian associations and activists (Fassin 2007).
Finally, the AIDS pandemic has highlighted what Vinh-Kim Nguyen calls the ‘triage’ of patients, at the intersection of state power, pharmaceutical companies and the expertise of caregivers (Nguyen 2010). In a context where there was a relative shortage of anti-retroviral treatments between 1994 and 2000 in the hospitals of Burkina Faso and Côte d’Ivoire, Nguyen shows how the healthcare teams conducted patient questionnaires to know which ones to treat most efficiently. Health workers decided who would get treated based on the patients’ performance during the questionnaire. In the wake of Michel Foucault and Giorgio Agamben, Nguyen calls ‘therapeutic sovereignty’ the right of life and death enacted by this practice. Similar protocols are now applied in the intensive care centres faced with an influx of patients from Covid-19.
The Ebola pandemic that developed in Guinea, then in Sierra Leone and Liberia between 2014 and 2015, confirms these lessons. The virus existed and still exists endemically in South Sudan, the Democratic Republic of the Congo, Gabon, the Republic of Congo and the Central African Republic, in the forest areas in contact with the virus’s animal reservoir, namely fruit-eating bats. In 1976, the disease made its presence felt to the rest of the world when it broke out in an epidemic in Nzara (South Sudan) and Yambuku (Democratic Republic of the Congo), near the Ebola River. The virus is transmitted by direct contact with biological fluids (blood, vomiting, etc.) and the mortality rate varies between 25% and 90%. At the start of the epidemic in West Africa in 2014, Western experts predicted a major disaster. Their predictions were contradicted by the facts. International aid, especially the action of African healthcare workers and local communities, controlled the epidemic, which infected just 28,646 people and killed 11,323 victims. The African medical teams and researchers, supported by equipment and volunteers sent by several countries and international institutions, succeeded in informing the population and implementing effective measures for observing and quarantining patients, and tracing contacts. They proceeded to rapidly organize emergency burials, build isolation clinics, and systematically disinfect laboratories and treatment rooms (Gomez-Temesio and Le Marcis 2017). In a major study, anthropologist Paul Richards demonstrates how the most effective eradication was led by African caregivers and experts in active liaison with the local population. On the contrary, where foreign teams acted alone, the fight against the disease ended in relative failure (Richards 2016).
Prejudice and history: interim findings on Covid-19
On 1 April 2020, French researchers Camille Locht (Inserm) and Jean-Paul Mira (head of the resuscitation department at Cochin hospital, Paris) discussed the advisability of testing a vaccine against Covid-19 in Africa, ‘where there are no masks, no treatments, no intensive care units’, and using prostitutes, ‘because we know that they are highly exposed and do not protect themselves’ (Sibille 2020). The following 10 April, Melissa Gates, the wife of the Microsoft tycoon, confided that she could not sleep at night for thinking about the likely impact of Covid-19 in Africa, and ‘the corpses that will soon litter the streets’ (CNN, 10 April 2020).
Not surprisingly, Covid-19 has brought out old stereotypes of an allegedly under-medicalized, pre-modern Africa where poverty and a supposed scientific underdevelopment condemn Africans to medical impotence. However, the history of epidemics and biomedicine demonstrates the long experience and extensive expertise of researchers, caregivers, and ordinary people. In addition, the experience of crises, especially health crises, is much stronger in Africa than in Western countries. What history and anthropology demonstrate is the importance of dialogue and mutual consultation between communities, experts and researchers in the social sciences, and the need to trust local understanding and strategies. The arrogance of wealthy, formerly colonial nations is not only historically unacceptable, it is medically and politically counterproductive. On the contrary, they need, as Helen Tilley says, to remember the importance of accepting the uncertain, of ‘not knowing’ (Tilley 2011), and to collaborate with the medical knowledge of Africans themselves (African Arguments 2020).
References
- African Arguments. 2020, https://africanarguments.org/category/covid-19-in-africa/.
- Arnold, David, ed., 1996. Warm Climates and Western Medicine: The Emergence of Tropical Medicine, 1500–1900, Amsterdam: Rodopi.
- Bernault, Florence. 2019. Colonial Transactions: Imaginaries, Bodies, and Histories in Gabon. Durham, NC: Duke University Press.
- Bigon, Liora. 2016. ‘Bubonic plague, colonial ideologies, and urban planning policies: Dakar, Lagos, and Kumasi’, Planning Perspectives 31 (2): 205–26.
- CNN. 2020. Interview with Melissa Gates, 10 April, https://edition.cnn.com/world/live-news/coronavirus-pandemic-04-10-20/h_0fdd34e7c008910ca58fec62fae049f6.
- Cohen, William B. 1983. ‘Malaria and French imperialism’, Journal of African History 24: 23–36.
- Curtin, Philip D. 1985. ‘Medical knowledge and urban planning in colonial tropical Africa’, American Historical Review 90 (3): 594–613.
- Echenberg, Myron. 2002. Black Death, White Medicine: Bubonic Plague and the Politics of Public Health in Colonial Senegal, 1914–1945. Portsmouth, NH: Heinemann.
- Fassin, Didier. 2007. When Bodies Remember: Experience and Politics of AIDS in South Africa. Berkeley, CA: University of California Press.
- Feierman, Steven and John Janzen, eds, 1992. The Social Basis of Health and Healing in Africa. Berkeley, CA: University of California Press.
- Gilman, Sander. 1985. Difference and Pathology: Stereotypes of Sexuality, Race, and Madness. Ithaca, NY: Cornell University Press.
- Goerg, Odile. 1998. ‘From Hill Station (Freetown) to Downtown Conakry (First Ward): comparing French and British approaches to segregation in colonial cities at the beginning of the twentieth century’, Canadian Journal of African Studies 32: 1–31.
- Gomez-Temesio, Veronica, and Frédéric Le Marcis. 2017. ‘La mise en camp de la Guinée: Ebola et l’expérience postcoloniale’, L’Homme 2 (222): 57–90.
- Hunt, Nancy Rose. 1999. A Colonial Lexicon of Birth Ritual, Medicalization, and Mobility in the Congo. Durham, NC: Duke University Press.
- Iliffe, John. 1998. East African Doctors: A History of the Modern Profession, Cambridge: Cambridge University Press.
- Iliffe, John. 2006. The African Aids Epidemic: A History. Athens, OH: Ohio University Press.
- Janzen, John M. and William Arkinstall. 1978. The Quest for Therapy in Lower Zaire. Berkeley, CA: University of California Press.
- Lachenal, Guillaume. 2014. Le médicament qui devait sauver l’Afrique. Un scandale pharmaceutique aux colonies. Paris: La Découverte.
- Livingston, Julie. 2012. Improvising Medicine: An African Oncology Ward in an Emerging Cancer Epidemic, Durham NC: Duke University Press.
- Lyons, Mary-Inez. 1992. The Colonial Disease: A Social History of Sleeping Sickness in Northern Zaire, 1900–1940. New York, NY: Cambridge University Press.
- McCullock, Jock. 2012. South Africa’s Gold Mines and the Politics of Silicosis Woodbridge: Boydell & Brewer.
- Ngalamulume, Kalala. 2006. ‘Plague and violence in Saint-Louis-du-Sénégal, 1917–1920’, Cahiers d’études africaines183: 539–65.
- Nguyen, Vinh-Kim. 2010. The Republic of Therapy Triage and Sovereignty in West Africa’s Time of AIDS. Durham, NC: Duke University Press.
- Niehaus, Isak. 2018. AIDS in the Shadow of Biomedicine: Inside South Africa’s Epidemic. London: Zed Books.
- Packard, Randall. 1989. White Plague, Black Labor: Tuberculosis and the Political Economy of Health and Disease in South Africa. Berkeley, CA: University of California Press.
- Packard, Randall. 2007. The Making of a Tropical Disease: A Short History of Malaria. Baltimore, MD: Johns Hopkins University Press.
- Pepin, Jacques. 2011. The Origins of AIDS. Cambridge: Cambridge University Press.
- Reynolds-Whyte, Susan, ed., 2014. Second Chances: Surviving AIDS in Uganda, Durham, NC: Duke University Press.
- Richards, Paul. 2016. Ebola. How a People’s Science Helped End an Epidemic. London: Zed Books.
- Sibille, Marie-Laetitia. 2020. ‘Coronavirus: Une séquence de LCI sur le test d’un vaccin en Afrique suscite l’indignation des internautes’, Journal 20 Minutes, 3 April 2020, https://www.20minutes.fr/sante/2754007-20200403-coronavirus-sequence-lci-test-vaccin-afrique-suscite-indignation-internautes.
- Summers, Carol. 1991. ‘Intimate colonialism: the imperial production of reproduction in Uganda’, 1907–1925’, Signs 16 (4): 787–807.
- Thomas, Lynn. 2003. Politics of the Womb: Women, Reproduction, and the State in Kenya. Berkeley and Los Angeles, CA: University of California Press.
- Tilley, Helen. 2011. Africa as a Living Laboratory: Empire, Development, and the Problem of Scientific Knowledge, 1870–1950. Chicago, IL: University of Chicago Press.
- Tonda, Joseph. 2002. La guérison divine en Afrique centrale (Congo, Gabon). Paris: Karthala.
- Trostle, James. 1986. ‘Anthropology and Epidemiology in the Twentieth century: A Selective History of Collaborative Projects and Theoretical Affinities, 1920 to 1970’, in C. Janes et al., eds, Anthropology and Epidemiology: Interdisciplinary Approaches to the Study of Health and Disease. Dordrecht: D. Reidel Publishing Company.
- Vaughan, Megan. 1991. Curing Their Ills: Colonial Power and African Illness. Cambridge: Polity Press.
- Webb, James L. A. Jr. 2013. ‘Historical Epidemiology and Infectious Disease Processes in Africa’, Journal of African History 54 (1): 3–10.
This article was first published in French by Sciences Po, Centre d’Histoire, Paris: http://chsp.sciences-po.fr/publication/quelques-enseignements-de-lhistoire-des-epidemies-en-afrique-florence-bernault?fbclid=IwAR19HL2a21vuxyOLBaHPFtsBzmgGVYk1XDxLd0qqVUOiKfaRLIpNViOXNnM.






