Can There Be A Democratic Public Health? From HIV/AIDS to Covid-19
As we are re-learning with the coronavirus pandemic, the outbreak and global spread of a novel disease, which has neither vaccine nor proven cure, causes panic. More precisely, it causes political leaders and communities to resort to behaviours that intensify confusion and anxiety. Meanwhile, despite expert assurances to the contrary, public health ‘best practices’ are at best well-informed projections with the uncertainty factors on mute. At worst they can be superstitions.
So it was with cholera in 19th century Europe, plague in colonial India, and the 1918-19 influenza epidemic when it ravaged the United States. In each case there was a rapid shift from denial and complacency to the imposition of authoritarian measures including cordons sanitaires, quarantine and isolation, forced slum clearances, and a host of restrictions that sometimes contained the epidemic, and sometimes made it worse. In some cases, those measures were so unpopular that they led to violent resistance such as the cholera riots of the 1830s. In other cases, poor people who faced starvation simply ignored or evaded the measures.
In eastern and southern Africa, the epidemics that arrived with the colonialists in the later 19th century caused social and demographic havoc, destroying some societies almost entirely, and giving rise to prophetic and millenarian cults elsewhere. Rinderpest ravaged cattle herds throughout north-east Africa in the late 1880s causing famine. Colonial public health was in turn often ideologically-coloured, racist and coercive, giving rise to enduring popular distrust of top-down medical policies. Contemporary historians have confirmed long-held suspicions that much imperial medicine was as much an agent of empire as of health.
At the turn of the millennium, as epidemic disease was recognized as a global security threat, it seemed that HIV/AIDS in Africa might bring entire societies to collapse, causing riots or revolutions. I was among those who feared for the worst. It didn’t happen. In fact, even while life expectancy plummeted and millions of households were thrown into distress, everyday life continued more-or-less as normal; people and politics adapted. In my African Arguments book, AIDS and Power, I asked why.
The first reason why AIDS didn’t lead to political crisis was that the epidemic did not intensify to the feared levels; high-prevalence countries such as eSwatini where HIV levels among adults reached over 30 percent, did not represent the future of other less-affected nations. The epidemiological models were too pessimistic—a problem that was later encountered in West Africa for Ebola, as described by Paul Richards and epidemiologically modelled by Yaneer Bar-Yam. Despite the vast amounts poured into AIDS research, some of the core epidemiological questions were never properly answered. For example there was never any systematic measurement of HIV incidence (new infections) as opposed to prevalence (total infections)—which is essential for accurate epidemiological modelling. Controversies about the spread of HIV by contaminated needles were never resolved. Most important, however, was that people changed their sexual behaviour to lower the risk. At the same time, anti-retroviral treatment became available and affordable.
A second reason why social crisis did not occur on the scale predicted was that predictive models were based on the accumulation of worse case assumptions and negative feedback loops, underestimating the resilience in society and the extent to which governmental institutions could lose human capital and still function. For example, the predicted bands of orphans roaming the streets never transpired, because family networks took care of them—at vast and unmeasured cost, no doubt, but nonetheless effectively.
Isak Niehaus has shown how an appreciation of local values and social systems was essential in dealing with the social consequences of the epidemic, especially care for orphans. There was no AIDS-related security crisis: senior army and police officers died of AIDS but they were replaced; protocols were worked out for HIV/AIDS among peacekeepers. The AIDS, Security and Conflict Initiative showed how the narrative shifted from predictions of global security crisis to the benefits of medical diplomacy. ‘New variant famine’ caused by the stress of AIDS in rural areas, outlined by Alan Whiteside and myself, did not transpire, as food systems and livelihoods proved resilient.
Isak Niehaus’s AIDS in the Shadow of Biomedicine- Published in association with @AfricaIai
Third, the disease was never the top concern of electorates. There were always more pressing political issues. Even in South Africa, this wasn’t the case. Without doubt there was huge political controversy: Thabo Mbeki’s denial that HIV caused AIDS and his refusal to implement public education and health measures that were standard elsewhere, sparked outrage. The Treatment Action Campaign staged large demonstrations and activists accused Mbeki and his ministers of genocidal indifference. But that didn’t appear to dent the African National Congress’s electoral performance. And, notably, the TAC wanted Mbeki’s government to reform, not to fall. Zackie Achmat and other TAC leaders tied their AIDS advocacy to other social issues such as housing and social services, and even at the height of their protests, regarded the ANC as their government, which it demanded should do better, not an enemy they wanted to remove.
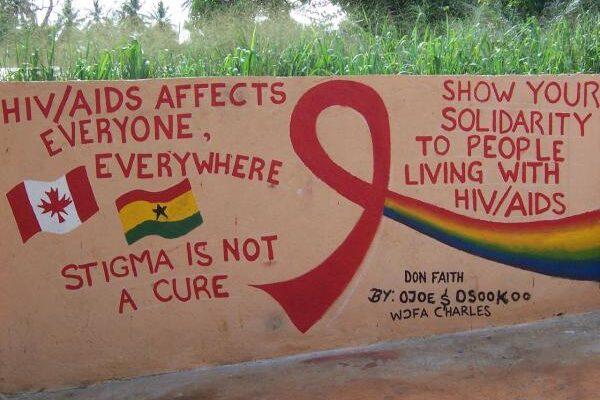
Perhaps the most important element in the politics of AIDS was the most unexpected. The global public health response supported human rights and civil society. Nothing like this had ever happened in the history of public health, where epidemic disease control has usually been organized on a military model and has been the occasion for intrusive state interference in people’s most private activities.
In a marked and novel contrast, the response of governments and international agencies (notably UNAIDS and the Global Fund to fight HIV/AIDS, TB and Malaria) was founded on principles of human rights. Civil society was consulted and often took a lead; people living with HIV and AIDS were embraced and even included in the governance structures of national and international responses; exclusion and stigmatization were denounced; gender equality and women’s empowerment were emphasized; principles such as strictly voluntary testing were insisted upon.
Africa’s response to HIV/AIDS wasn’t conventionally liberal. In fact, some of the most effective responses were in countries that were authoritarian, such as Uganda and Zimbabwe. What they had in common was that governments took the lead from community organizations and encouraged local programmes and practices. There was a vast apparatus of interactive workshops, learning-by-doing, critical public debates, participatory appraisal methods—frustrating and inefficient to those who were convinced that they already had the right policy prescriptions which just needed to be implemented properly, but essential in creating the kinds of plural, uneven consensus that was needed to combine people’s science with expert science.
The inclusive response was particularly remarkable in that AIDS was a sexually-transmitted disease, associated with stigmatized groups, which remained incurable until well into the pandemic. Did this represent a new, more democratic paradigm for global public health? Jennifer Chan has argued for the potential of this emancipatory model in not only in tackling infectious disease but also in promoting progressive social change. I lean towards this view, from both experience and optimism. But we must be alert to alternative readings too. Peter Baldwin is sceptical about the likelihood of democratic public health: ‘In the era of governmentality, public health remains one clear area of statutory control where the average law-abiding citizen might expect to feel the iron first through the velvet glove.’ Today we face the paradox that contemporary health governance has individualized responsibility for remaining infection free, while states have accumulated greater-than-ever powers of surveillance and control.
As coronavirus transmission enters its exponential phase, does Africa’s experience with HIV/AIDS have anything to teach us?
Trying to ‘learn lessons’ from one public health crisis to apply to another is a problematic exercise, so we should be wary. There are as many lessons as commentators; writings on crisis often reveal more about the writer’s other preconceptions as about the events at hand. As Hans Steinmuller observes in an introduction to anthropological writings on Covid-19, ‘Propelled by the urgent necessity of crisis response, everyone thus takes us on a ride on their hobby horse.’ Horrified by the Trump Administration’s hostility to science and by the austerity-driven cutbacks to public health provision in the UK, it is tempting to celebrate medical authorities as the fount of wisdom. But expert models for epidemics are based on data points that are as-yet-unsubstantiated and framed by readily-obscured ideological precepts. There is in reality little certitude in public health authorities and their prescriptions. And decisions made at the height of a public health emergency will have ramifications far beyond the moment—and far beyond public health itself.
Africans do, however, have hard-earned experience of epidemics and other life-threatening crises, and two general observations are in order.
First and most important: critical thinking is always needed and especially so at times of crisis. When scientific policy is at its most fragile and when momentous decisions are being made, it is especially important to be consultative and open-minded and resist the pressure for an authoritative closure of debate. Two, public health and inclusive politics are well served by partnership. As the coronavirus pandemic unfolds, citizens in Africa and industrialized countries are being asked to place their trust in science—without science reciprocally placing its trust in the wisdom of a questioning public. As an issue of both principle and practical outcome, that should be questioned.
Africa’s experience with HIV/AIDS and other epidemic diseases and their (mis)handling shows that consultative and inclusive policymaking is essential for the health of both people and democratic society.







