Debating Ideas is a new section that aims to reflect the values and editorial ethos of the African Arguments book series, publishing engaged, often radical, scholarship, original and activist writing from within the African continent and beyond. It will offer debates and engagements, contexts and controversies, and reviews and responses flowing from the African Arguments books.
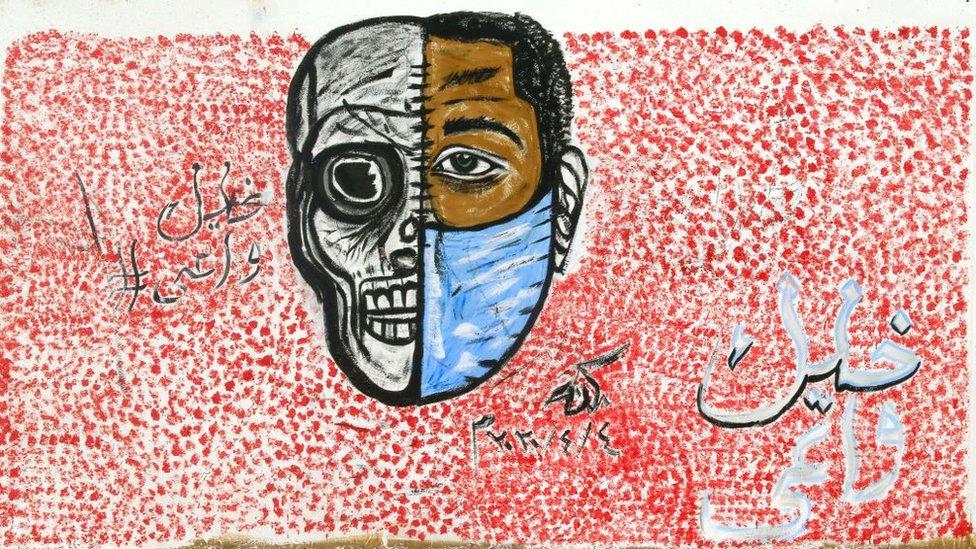
Art for public health campaigning in Sudan illustrates the relationship between prevention and surviving Covid-19.
Covid-19 comes in waves
Much thinking about Covid-19 has been dominated by influenza as a model disease. Flu viruses mutate rapidly, and every season there are potentially new strains – some more nasty than others. It is next to impossible to prevent flu, since it spreads very effectively among children at school. Without a vaccine, cases rise exponentially, and only fall away as herd immunity builds up in the population. The dream of flu-like herd immunity still captures the attention of some epidemiologists and policy makers in relation to Covid-19.
It is now increasingly evident, however, that Covid-19 is not like flu (Scoones 2020). The WHO was quick to articulate the advice to damp down the initial wave and build an effective rapid-response system of ‘find, test, trace, isolate and support’ (FTTIS) to deal with further outbreaks once the overall number of cases was reduced. The organization warned that without constant attention to local outbreaks there would be a second wave of the disease. This second wave has now begun to hit most European countries. The reasons are not yet fully established. Apparently, governments and citizens took their eye off the ball during the summer break. Thinking in terms of flu, too many people assumed life was returning to normal, and began to behave in ways that accelerated the spread of the disease. Due to limitations of FTTIS, we often do not know how, where and why people are being infected accurately enough to stamp down on the disease without disruptive lockdowns.
UK is fast becoming one of the countries in Europe worst affected by the second wave, and this is because it failed during a summer downturn to develop an effective system of FTTIS. The government is still wedded to a ‘telephone sales’ model of contact tracing run by private-sector providers. The system is too centralized and focused only on ‘forward’ tracing (dealing with cases of people in contact with a known case). Contract tracing in Germany has been better, since it is more fully localized. Here, there has been some attempt at ‘backward’ tracing (following infection chains to their source). This potentially provides vital information on how and where people are becoming infected, in order to provide pointers to activities serving as super-spreaders. But this backward tracing has to be done early enough, when case numbers are low. Once an epidemic builds momentum contact tracing is overwhelmed. Knowledge of infection pathways through contact tracing enables a more targeted response to suppression. Targeted rapid response helps avoid need for a later general lockdown. There is wide agreement that the economic and psychological side-effects of general lockdown are too severe.
Managing second waves, however, requires improved understanding of the causal mechanisms involved in infection chains – what, for example, are the relative risks of infection associated with working in a packing plant or clothing factory, compared to drinking in a bar or taking part in a church service? Much of this understanding is situation-specific. For Africa, a factor on which currently we have too little comparative information is the importance of ventilation. The virus is carried in fine particles in the air and dispersed by breeze. Many daily activities in poorer tropical Africa take place in the open air, or in well-ventilated environments such as open-aided sheds providing shade, and this may be a factor in lower transmission rates for SARS Cov-2 virus.
Better understanding of infection dynamics requires a better mapping of key social processes. French health authorities, for example, are explicit about a weakness in their contact tracing – that insufficient attention was paid to festive activity in the domestic sphere. Domestic celebratory gatherings may be equivalent to funerals during the West African Ebola crisis – social events not readily subject to infection control, and thus serving as super-spreader events. This points to a failure to incorporate relevant areas of social knowledge in Covid-19 response. We know from Ebola in West Africa in 2014–15 that funerals were key super-spreader events but that epidemiologists were not well equipped to understand funerals and had to turn to anthropologists for help.
The same may now be true of Covid-19. In Britain, rather few anthropologists are present in scientific advisory groups shaping Covid-19 response. Could it be that this has hindered responders in working out the relative importance of ceremonial activities, especially in the family setting, thereby depriving response initiatives of specific knowledge to modify key areas of social activity driving infection?
Preparing for a second wave of Covid-19 in Africa?
A capacity to target and control infection risks without disrupting social interaction more generally is a key theme for Africa as well as Europe. It is crucial to assessing how well Africa is prepared for a potential second wave. The prediction that Covid-19 would hit Africa even harder than Europe or North America, due to general levels of poverty and the inadequacies of health care, has not been borne out. Up until 12 October 2020 there have been just under 1.6 million cases of Covid-19 in Africa, with 38,396 deaths, with a large proportion of cases associated with just three countries – Egypt, Morocco and South Africa. For comparison, the fifteen countries of West Africa have experienced only 181,600 cases and 2,662 deaths. The figures for eastern Africa are similarly low. Perhaps because of a prompt response, or perhaps because of factors not yet fully appreciated, such as a greater proportion of activity taking place out of doors, African countries succeeded in damping an initial wave.
However, European experience shows that second waves of Covid-19 can be worse than the first. Africa should not rest on its laurels, especially when we do not know as yet why the initial figures were kept relatively low. In Europe the second wave began when countries began to think they had seen the back of the disease. Like flu, it was presumed to have just disappeared (to paraphrase the President of the US). Africa should avoid that mistake. The way to avoid a second wave, before vaccines or cures become available, is to ensure that cases remain low, which means monitoring and jumping on local outbreaks as soon as they occur. If cases surge, even the best organized contact tracing system will be overwhelmed, and (as in Britain and France) lockdowns will inevitably return, even if thinly disguised as ‘circuit breakers’ or ‘tiered’ responses.
Two things are required, and now rather than later. One is to invest in rapid testing. This depends on new technical advances in testing that seem likely to become available in the near future. The current standard is a test that is both expensive and requires time (24-hour turn-round is about the best that can be achieved). What is needed are tests taking perhaps no more than 15-20 minutes, costing only a fraction of the existing gold-standard laboratory polymerase chain reaction (PCR) swab tests. Such new kinds of cheap and rapid tests are about to become available and are reviewed below. Like Ebola, Covid-19 infection takes places in clusters. These new tests are potential game changers in being potentially able to identify infection clusters before they get out of hand.
The second requirement is to apply the process of contact tracing in such a way that it generates better, more accurate social awareness of the contexts in which the disease is spreading, to ensure that control measures are targeted and proportionate to the infection risks involved. This is not simply a matter of knowing that funerals spread Ebola, or that birthday parties and weddings spread Covid-19. Any curtailment of social activities can only be attempted with the willing cooperation of the groups affected. It must be regulation by consent, and (better still) with the active social involvement in infection management of affected populations within the cluster concerned.
Communities must be convinced that the infection risk is real and that their own actions will be effective in achieving control over the disease. This was a lesson learned in the recent large-scale Ebola outbreaks in Upper West Africa and north-eastern Congo. Any African action to curtail a second wave of Covid-19 should be based on that approach. It requires facilitators to be grounded in a good knowledge of how communities think.
Managing an African second wave – rapid diagnostic tests
If there is a second wave in Africa, rapid testing will be a key to its management. Here, we provide a short review of the kinds of molecular tests currently available or under development as well as some lower technology tests that could also be useful (including use of dogs).
The three main targets for testing for Covid-19 are: 1. (SARS-CoV-2) viral RNA; 2. the proteins of an intact, functional virus – e.g. the spike, membrane, nucleocapsid, and envelope proteins (there are over 25 other proteins expressed during infection); and 3. human antibodies (mainly IgG and IgM classes) to viral antigens. The three main classes of tests, then, are nucleic acid tests, antigen tests, and antibody tests. All of them have restrictions in application and appropriate timing, which affect their usefulness, whether the purpose is diagnosis or epidemiological control: stopping transmission, reducing transmission, maintaining viral ‘free’ zones, public health or community surveillance.
A typical graphic of probability of detection by test class shows nucleic acid tests with the broadest range of detection, from some days before symptom onset to over three weeks later, antigen tests with a narrow window from less than a week before to less than a week after symptom onset, and the (humoral) human antibody response, detectable by antibody tests, peaking about two weeks after symptom onset, with IgG antibodies staying higher while IgM detection falls off more rapidly (Guglielmi 2020).
A large portion of transmission occurs before symptoms are noticed, in patients who become observably ill. About 40% of people who are infected show no noticed symptoms and are considered asymptomatic, yet account for about 50% of viral transmission. It can be an epidemiological disaster, when testing is solely based on detected symptoms — in particular when there are contacts with known significant exposure but these contacts are only tested if themselves showing (sometimes multiple) symptoms.
There is a basic conundrum for testing methods: the slowest, most expensive, laboratory intensive, and supply-chain sensitive – nucleic-acid tests – are the best both in general and for detecting asymptomatic carriers over a broad window of time. The antigen tests, which can be used for cheap and rapid mass screening only have a chance of detecting asymptomatic carriers in a very narrow window of time; and that window, at best, can only be guessed at from the history of exposure to a known symptomatic patient. This can be excellent as part of contract tracing, isolation and transmission control, but hit or miss when there is community transmission. Used incorrectly they can be misleading or dangerous. There are two WHO affiliated international consortia for Covid-19 testing (and drug development) and vaccines. These are the Access to Covid-19 Tools (ACT) Accelerator (1), and the COVAX Facility (2), respectively. The great majority of countries (or economies) in the world, by numbers, are included in the consortia. However, three nations that are not participating are China, Russia and the USA.
On September 28, 2020, WHO announced that 120 million ‘affordable, quality COVID-19 tests for low- and middle-income countries’ would be made available. Africa CDC will be one of the agencies handling test introduction. These are point-of care, antigen tests made by two companies: the Abbott (USA) Panbio™COVID-19 (antigen test) and the SD Biosensor (South Korea) STANDARD Q™COVID-19. The WHO affiliated Foundation for Innovative New Diagnostics (FIND) released a report on the SD Biosensor test on 18 September 2020. Comparison is made to diagnostic qRT-PCR[i] for analytic or diagnostic sensitivity and specificity.
Most pharmaceutical test manufacturers are on the second or third generation of their tests. One might hope that a test intended for millions or hundreds of millions of uses would have as much testing before use as a drug or vaccine. But the need exceeds the time available. Many tests require reading by proprietary equipment using proprietary chemistry, which are susceptible to supply chain disruption, as the UK NHS found in early October 2020 when supplies from Roche were disrupted. Most actual tests should have a black-box warning about their correct use and interpretation, but do not.
Ideal new tests might include (1) a cheap nucleic acid test based on saliva or cheek swabs and read at home or point-of-care like a semi-quantitative pregnancy test (number of lines varies by concentration); (2) cheap accurate measures of components of cellular immunity (not just IgG and IgM) over time; (3) safe and effective measurement of intact, infectious virus; (4) tests that can accurately identify asymptomatic or pauci-symptomatic individuals with mild symptoms, as-yet unknown symptoms, or no symptoms but who are infected and can transmit to others.
Research on new methods of detection and reporting for all classes of test changes by the hour; often with the possibility of vast improvement in accuracy, resilience against viral mutation, use near point-of-care, no dependence on proprietary chemistries for field use, ease of use without training, easier sampling, and low cost. An entire recent issue of Biosensors and Bioelectronics is dedicated to Covid-19 diagnosis technologies. For example, one article describes developing direct optical measurement, without sample preparation, using a spike protein specific Nano plasmonic resonance sensor within 15 minutes.
A dog might ask, with some justification, ‘why don’t you just smell the disease?’ Human limitations of smell are notorious (Goodman and McGregor 2010), but dogs have been trained to report for rescue, recovery, drug detection, bomb detection, land mine detection, the plant disease causing (the horrendous) citrus greening and other uses. Training of dogs for Covid-19 detection and reporting is ongoing in, among other countries, France, the Netherlands, Germany and Finland. Helsinki airport currently employs trained Covid-19 detection dogs. A modest sized clinical trial of test comparison with qRT-PCR diagnosis has been made in France. Dogs are not exposed to direct contact with potential disease carriers; instead, samples are brought to them in a separate room, usually of wipes of sweat.
Only qRT-PCR community sampling could generate human samples of pre-symptomatic or asymptomatic yet infected individuals to see if dogs could detect them as well. And if not dogs, with 10,000 to 100,000 times human capacity for smell, then one of the giant African rat species with 10,000 times dogs’ sense of smell. African giant pouched rats are being trained in Belgium, Tanzania and elsewhere for detection of land mines, or tuberculosis. Detection instruments might be developed to match these capacities. These could be similar to military and national security instruments for detecting chemical, biochemical or pathogenic agents or, in contrast, for more routine sampling of foods. The main targets, presumably similar to detection by dogs, would be the volatile organic compounds released by the disease-patient interaction phenotype (Calvo-Henriquez et al. 2020).
There are unique signs or symptoms (narrow sense) for some diseases that can carry a kind of signature when found. For first detecting Ebola in West Africa, a key sign (observable), in some patients, was hiccupping. For Covid-19 a key symptom (reported by the patient) is loss of sense of smell and taste. The self-reporting can be improved upon, and become semi-quantitative, and observable, by testing patients using a series of ethanol dilutions on swabs. The authors of this cited article aimed ‘to develop and validate a fast, inexpensive, reliable, and easy-to-perform olfactory test’ for screening suspected cases of Covid-19. Covid-19 has also presented the unusual contrast between patients who speak normally, are not reporting breathing issues, but have low oxygen saturation and severe symptoms (broad sense) of lung damage.
Dedicated pulse oximeters measuring oxygen saturation can be very useful objective measures for early identification of patients. They may be rarer in Africa but are being incorporated into smartphones. This could be required for all new models, thus establishing baselines for uninfected people and acting as a warning when oxygen saturation drops. Finally, a singularly effective and efficient epidemiological use of qRT-PCR is for sampling of water treatment facilities, sewer systems, or plumbing (where these exist) which allows identification of cities, neighbourhoods, and individual buildings where Covid-19 is present (usually as non-infectious ‘debris’).
Preventing transmission, even before testing, is critical. The single most important change in behaviour is prevention of transmission by wearing face masks, followed by social distancing, and hand washing. Many kinds of face masks can reduce transmission from an individual. Increasing improvement in availability of better face masks can ultimately reduce transmission to individuals as well. Quantitatively-fitted medical N-95 masks are an example of this. So the provision of improved qualities of masks to the population should be a high priority, with the most protective going to the most exposed front-line workers. These can be supplemented by face shields. Environmental and social contexts with high probability of transmission should be avoided, where possible; or the conditions can be modified to lower the probability of transmission.
This brings us back to the social epidemiology of prevention, detection and control, and the importance of investing in a human skill – contact tracing.
Managing a second wave in Africa – backward contact tracing
Contact tracing is, in the first instance undertaken to identify, isolate and support infected persons. If done in the right way (namely, including backward as well as forward tracing) it is also an important tool for responders (including communities) to learn how Covid-19 moves, and thus to enable risk reduction through targeted pre-emptive action. Currently, quite a bit is now known about the settings in which clusters of Covid-19 infection form. In Europe, outbreaks have been linked to specific kinds of production or residential settings, such as meat-packing plants, fruit farms, student dormitories and care homes for the elderly. These sites of risk are identified by backward contact tracing – enquiring how and where patients testing positive for the virus might have become infected.
In the West Africa Ebola epidemic medical admission forms asked whether the patient had recently attended any funerals. This information confirmed that funerals were events carrying high infection risks. But they didn’t reveal what aspects of attendance at a funeral conveyed the risk. That required ethnographic enquiry into how funerals were conducted. It transpired that it was not funeral attendance that caused the hazard but the processes of body handling involved in preparing the dead for burial. This was activity that fell especially to older members of the family of the deceased. Few family members were willing to allow a burial to proceed unless the corpse was properly cleaned. Ways had to be found to perform this essential task safely. Data were needed on survival times of the virus on dead bodies and as fomites on bedding, for example. To our knowledge, the survival times of Ebola virus on soiled bedding hauled into direct sunlight are still to be ascertained.
In the European instances of Covid-19 infection mentioned above information is needed on the more exact configuration of risks in factory, farm and group residential settings. With meat packing plants it may be working together in poorly ventilated conditions that transmits the disease, whereas on fruit farms it may be collective feeding of workers rather than outdoor work picking fruit that constitutes the infection event. In old people’s homes a key factor in infection transmission may be the casual and multi-site nature of poorly-paid work, where carers can neither afford to take time off sick or give up multiple jobs.
There are two points for Africa. First, a lot of what is known from Europe and elsewhere may not be relevant to understanding Covid-19 infection risks in Africa. Crowded markets and public transport may be much more important sources of infection than factories or residential homes for the elderly.
Secondly, as with funerals and Ebola, we need to know much more about the way infection hazard is shaped by key ceremonial activities in private spaces. African elders play a part in communities after death, and events such as 40-day and one-year memorial ceremonies may pose more significant exposure risks for Covid-19 (because they gather together a wider group of mourners from a greater distance) than the funeral itself. Backward contact tracing, in other words, requires active and sensitive social enquiry far beyond the form filling of a kind that can be entered into a computer.
While these kinds of anthropological data are being compiled there is also a need to enter into local dialogue about what can be changed, and how. With funerals under Ebola, people accepted draconian controls (e.g. burial by trained burial teams dressed in biohazard suits) only when some of their own concerns had been addressed, such as a requirement for a pastor or imam to officiate as the burial team did its work, and the need for the family to witness the interment, even if from a distance.
There would need to be similar negotiations over post-burial memorial events. Attempts to suspend 40-day ceremonies might be as unsustainable as lockdown closure of churches and mosques. The longer-term solution might be to assess more exactly where the hazard lay, and to work round it, with the help of such things as face masks and socially distanced seating plans.
This is where the ability rapidly and cheaply to test people attending such events might prove to be a major boon. Consider the dilemma of younger people exposed to Covid-19 infection risk not being sure whether they can visit elderly and frail parents for fear of infecting them with a disease that might well be a death-sentence. A cheap and rapid test would provide re-assurance that such essential and mundane family interactions were safe to undertake. Under Ebola, in Sierra Leone, people used to reassure each other ‘I know my status’ (i.e. I have been tested negative for Ebola). In other words, social consciousness of the risks of spreading the disease was high.
Rapid, reliable, low-cost testing for Covid-19 would serve a similar socially liberating purpose, when used appropriately, and the good news is that many different possibilities are being developed. African countries should watch developments very closely and seek to access the technology as soon as available, even while the risk of a second wave is not yet fully apparent.
Some recent research suggests that African communities quickly formed an effective knowledge of the risks posed by Covid-19 during the first wave, even though the disease was far less visible than Ebola ever was (Kamara et al. 2020). This confirms that it would make sense to involve at-risk communities of all kinds in debate about how to manage the hazards associated with a second wave of the disease in Africa, based on diligent backward contact tracing undertaken while disease circulation remains relatively low. The time to do this work is now. If a second wave arrives it will be too late.
Endnote
[i] This stands for quantitative reverse-transcriptase polymerase chain reaction. The ‘RT’ part allows an RNA sequence to be amplified.
References
Calvo-Henriquez, C., Maldonado-Alvarado, B., Chiesa-Estomba, C. et al. 2020, ‘Ethyl alcohol threshold test: a fast, reliable and affordable olfactory assessment tool for COVID-19 patients’, European Archives of Oto-Rhino-Laryngology 277(10): 2783–92. doi:10.1007/s00405-020-06131-3
Guglielmi, G. 2020, ‘Fast coronavirus tests: what they can and can’t do’, Nature, Sept 1, 585 (7826): 496–8.
Goodman, L. E. and McGregor, R., translators, 2010, Epistles of the Brethren of Purity [Ikhwan al-Safa]: The Case of the Animals versus Man Before the King of the Jinn [late 4th Century AH, 10th Century CE]: An Arabic critical edition and English translation of Epistle 22. Oxford: Oxford University Press.
Kamara, F. M., Mokuwa, E. Y. and Richards, P. 2020, ‘How villagers in central Sierra Leone understand infection risks under threat of Covid-19’, PLoS ONE 15(6): e0235108. https://doi.org/10.1371/journal.pone.0235108
Scoones, I. 2020, ‘Science, uncertainty and the COVID-19 response’, https://steps-centre.org/blog/science-uncertainty-and-the-covid-19-response.